Welcome to the New Inclusive Patient Participation Forum.
We are trialling a new format for patient engagement and dissemination of news and the gathering of your views. We have divided the newsletter into sections and will be requesting feedback on each of the sections and there will also be the opportunity to put in ideas for improvements. We want to explore ACCESS in this issue.
We have opened up this opportunity to all of our patients and have sent electronic invitations to 17,000 of our patients. If there are patients who have not received this invitation because we do not have an up to date mobile telephone number, please can you get them to contact the surgery to update our records and request the link. There will be a paper copy to read at reception for those who do not have access to mobile phone or the web site. The integrated survey is an electronic survey via Survey Monkey. The surgery serves the whole community and we need to hear from everyone.
We need SMART suggestions:
S specific
M measurable
A achievable
R realistic
T timely
I am afraid the usual social media commentary of “they are rubbish” and “they should be shut down” is unhelpful, and does not meet any of the SMART criteria. It does not tell the surgery which site is preferable to access if you are a wheelchair user, or what measures would help patients to access care with varying degrees of vision, hearing or cognitively impairment? We are changing how we do things all the time, constructive suggestions to improve healthcare for all are always welcome.
News:
We were hoping to confirm exciting news about NEW PREMISES, but solicitors are still dotting “i’s” and crossing “t’s”, we hope to announce this and give more details in our next issue. In the interim we need to know how different groups are coping with accessing each of the sites, given that none of our sites were purpose designed and built, FOR DISABILITY ACCESS. See access section and respond on the Survey.
This issue has a detailed explanation of our APPOINTMENT SYSTEM and how it compares to other surgery’s in Sussex.
There is an update on The TELEPHONES and ONLINE CONSULTATIONS.
The most exciting section is the INNOVATIONS section.
Appointment Comparative data
Booking GP appointments is the single most important issue for patients, when asked about GP services. So what follows is an in depth explanation of our appointment system, how and why it evolved and how it compares with other surgeries.
All GP appointment data has been mapped and analysed, and nationally compared, for a few years now. The analysis is ever more in depth.
The Sussex Integrated Care Board (ICB), who commission healthcare from hospitals as well as general practice , have prepared appointment data analysis for The Hill Surgery in response to an external enquiry, which they have shared with the surgery:
In 23/24 The Hill Surgery delivered 782.4 appts per 1000 ptns, ranking the 5th highest in Sussex (Sx average 498.9 per 1000 ptns) and 2nd Highest in East Sussex (ES average 536 per 1000 ptns).
(This is an average per month figure, and equates to an average of just over 9 appointments of all types, per person, per year, across the whole team, which is in line with what we have been providing for a few years now. Of course, on an individual basis the average is meaningless. There is a wide variation in attendance rates between those patients that don’t contact the surgery for years, and those that feel they need to access our services several times a week, so the average per 1000 is just a standardised capacity figure for comparative purposes.)
In order to provide sufficient access, all GP appointments will be managed by telephone first. There will be no directly bookable face to face GP access, unless reviewed and triaged by telephone first. Nurse appointments are available to book in advance by telephone.
According to GPAD data The Hill Surgery offered:
- 38.5% of patients face to face in 23/24 ranking 147 out of 156 practices, the Sussex average was 67.7%.
(as we are providing 283.5 more appts per 1000 pts than the average, per month, ie 56% more, we are providing nearly as many face to face surgery appointments , but also far more other types of appointment to maximise use of resources and increase access)
- 66.9% of patients were seen on the same day appointments in 23/24 ranking highest in East Sussex average 45.5% and 2nd highest with the Sussex average of 42.2%.
- 91.2% of patients were seen within two weeks in 23/24 ranking highest in East Sussex average 80.6% and 8th highest with the Sussex average of 78.9%.
Online appointment booking is now available, subject to availability, through the NHS App / Patient Access portals.
Many of our patients do not understand “why can’t I just ask to see a GP like I use to?” The answer is diversity of supply and demand management. If you are interested in why we have a total triage system we will explain how this evolved in detail, if not, you may want to skip ahead to the innovations section.
Every conceivable way has been tried since the NHS was formed to get the supply of GP time available to match the demand. There was never a time when general practice could supply sufficient doctor appointments to accommodate all demand.
The early surgery format up until 40 years ago was an open surgery system in the morning, where you had to get up early, miss work and just come and sit and wait for on the day problems, sometimes for several hours, demand was managed by how exasperated you were with the wait. The average appointment time pre 1995 was 6 minutes with GPs seeing over 40 patients per day.
When Tony Blair was accosted about GPs being booked up many days in advance as they were running all booked appointments, with only a couple of urgent on the day appointments, the political push was then to turn this on its head, and book only a couple of appointments in advance, and everything else on the day. Tony was able to announce millions more on the day appointments. This was usually booked by phone between 0830 and 0835, after that it was “phone back tomorrow”, the appointments 25 years ago were on average 10 minutes as we had started doing more opportunistic health screening and many more effective drug treatments and investigations were becoming available in general practice. GPs were seeing about 30 patients per day. At this time, the average number of booked appointments provided was around 3 per person per year.
Since then, the UK population has become older, sicker and more complicated. Before 1986, if you had a heart attack, you were put on bed rest, and the doctor popped back 2 weeks later to see if you were still around! Now cardiologists do amazing things with stents and revascularisation and cardiac patients are on around 8 medications. These all need monitoring and adjusting to get blood pressure down, and blood tests done for getting cholesterol etc to target, in general practice, often with ecg screening.
25 years ago there were thought to be an average of 1% diabetics, and another 1 % we hadn’t found, diabetes was largely a hospital managed condition, first presentation was quite late in the disease. With active screening, we now have 8% diabetics (as a percentage across all ages) and 7% pre diabetes, with a plethora of medications to adjust and monitor, including insulin that is started and monitored in general practice.
So the question should not be “why can’t I just ask to see a GP like I use to?” but “how does general practice do all this, while offering an average of 9 appointments per patient per year?” Considering that face to face appointment times are now on average 15minutes or more due to the complexities and the number of the conditions we are managing, and BMA safe working guidance is now 25 appointments per day.
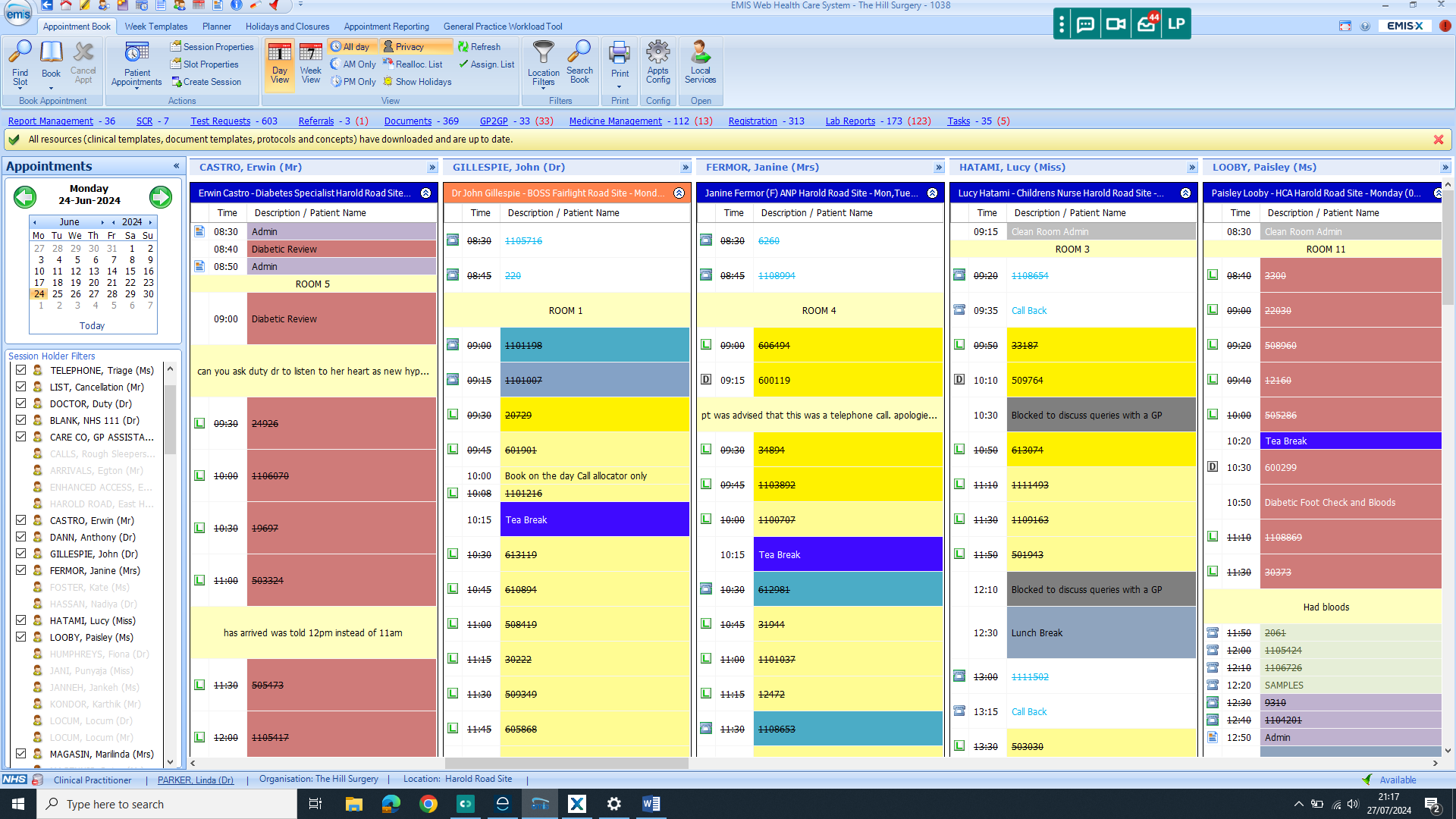
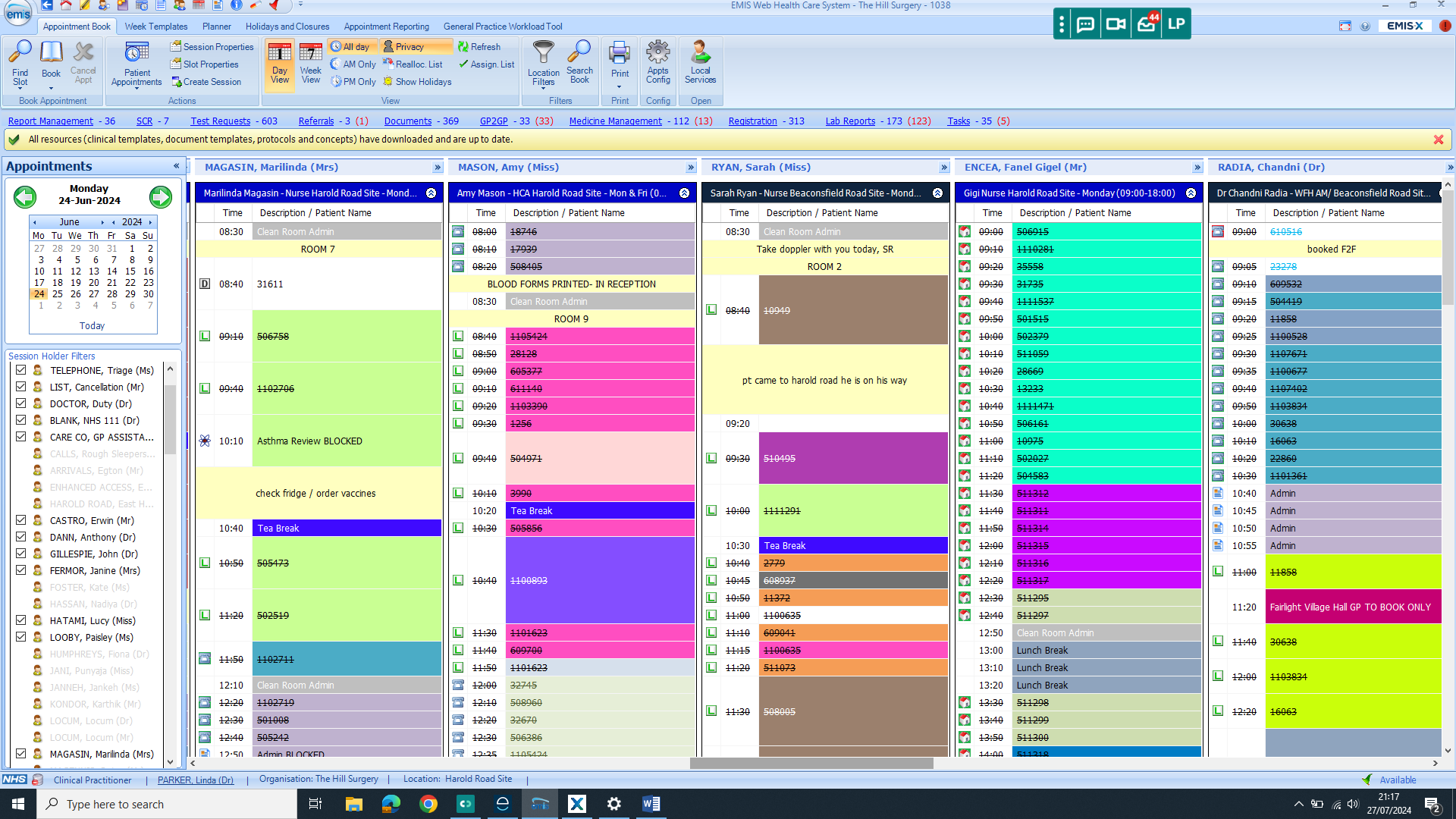
The answer is of course diversity of supply of appointments and triage to the multidisciplinary team. It is not just doctors who deliver the care for the surgery, but nurse practitioners, specialist nurses, practice nurses, health care assistants, physiotherapists, paramedic practitioners, clinical prescribing pharmacists, general pharmacists and medication management technicians that have allowed the expansion of general practice and the tripling of demand for access over the past 20 years. Clinical space is very limited at the surgery, and it is not unusual, particularly on a Monday for all of our available rooms to be occupied with clinicians and up to 6 doctors doing calls and online consultations tucked away in administrative offices. Technology has allowed for our team to be expanded without having to find more consulting rooms and the remotely located doctors and pharmacists work form London and Cambridge, some overnight when the surgery is closed, to process online consultations, prescription requests and results. Not everyone wants to take time off of work to attend in person, or spend £10 on a taxi to the surgery, phone and online consultations suit many patients with conditions that do not require a physical examination.
We have also been offering extended access appointment for many years, which are all pre bookable, out of the usual surgery core hours. We struggle to fill these pre booked appointments on Tuesdays and Thursdays evenings every week, and one Friday evening and a whole day on a Saturday once a month.
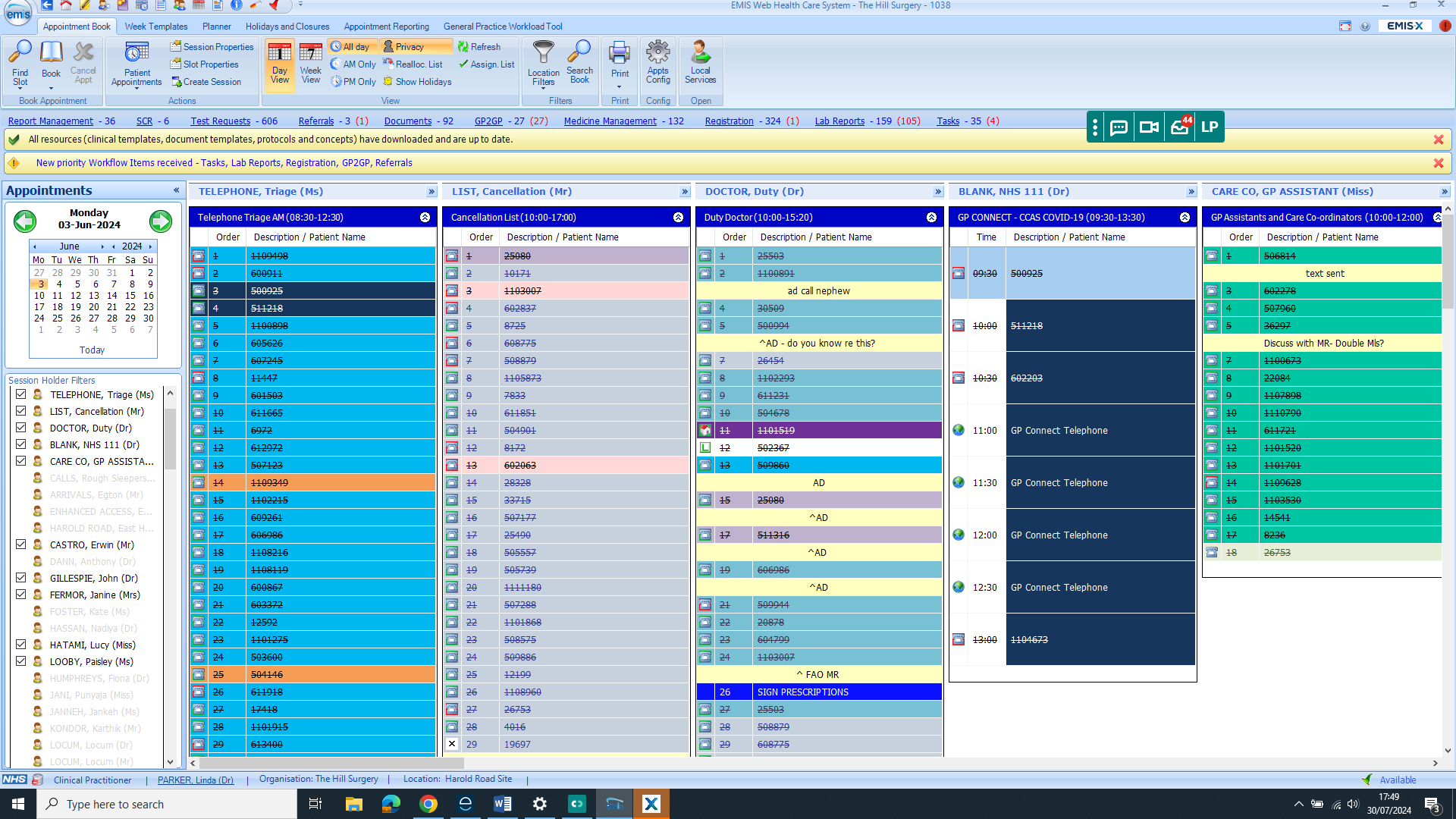
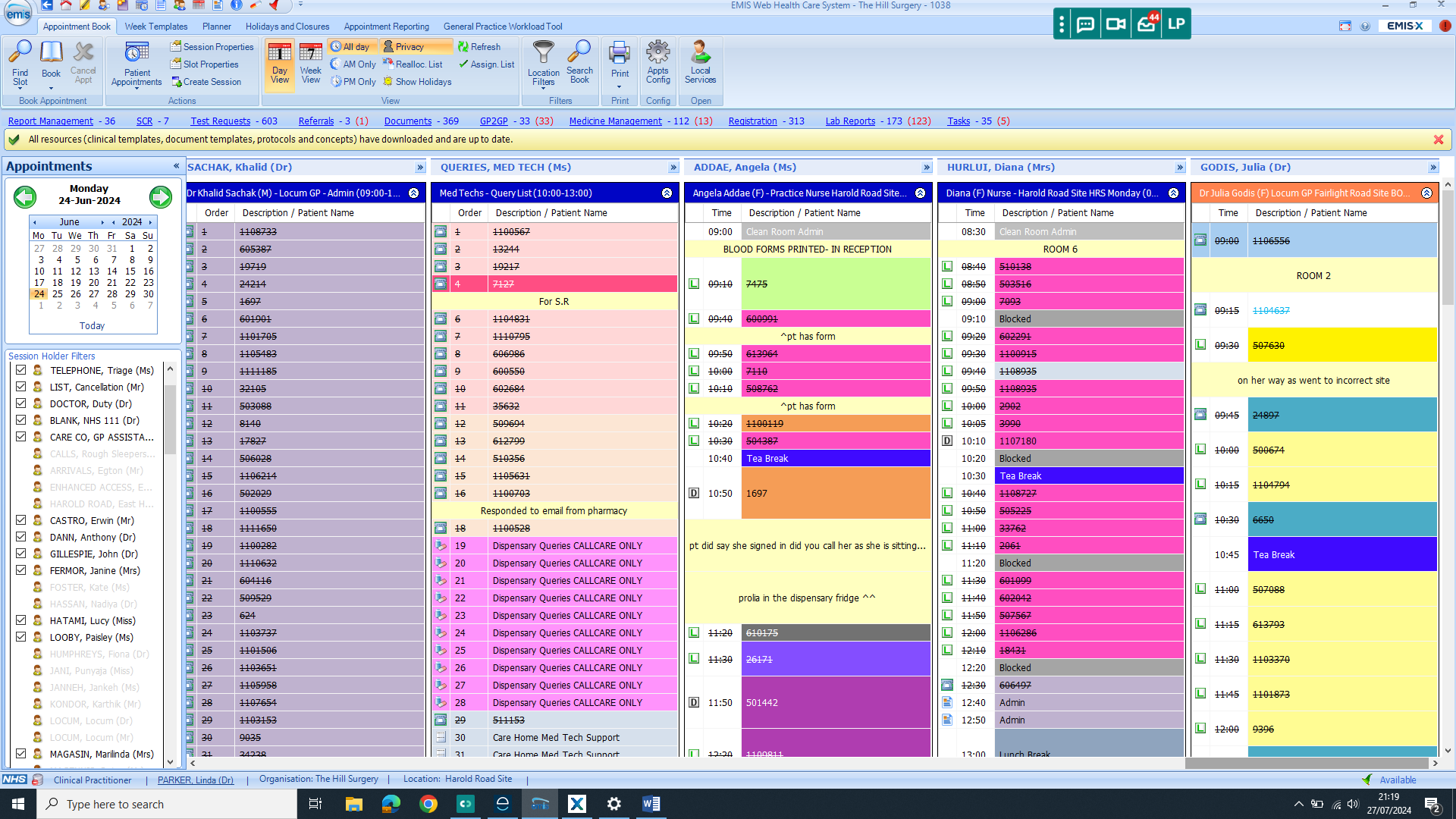
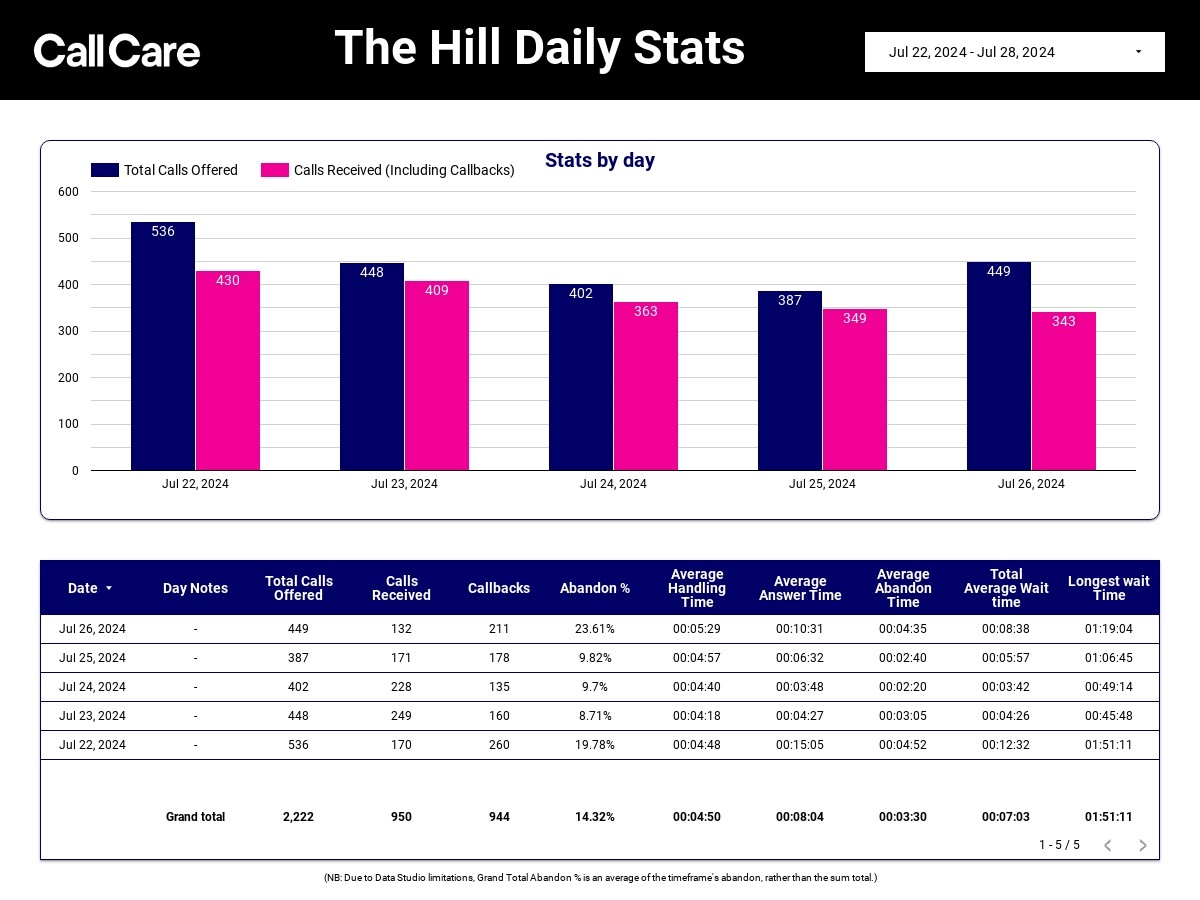
The 5 Appointment screen shots are the start of the day for Hill Surgery, the actual list lengths are far longer, but vary depending on the type of clinician and appointment. The first 3 lists are 120 to 180 patients. Just to show we are not just sitting around drinking cappuccinos, as some media voices would have you believe.
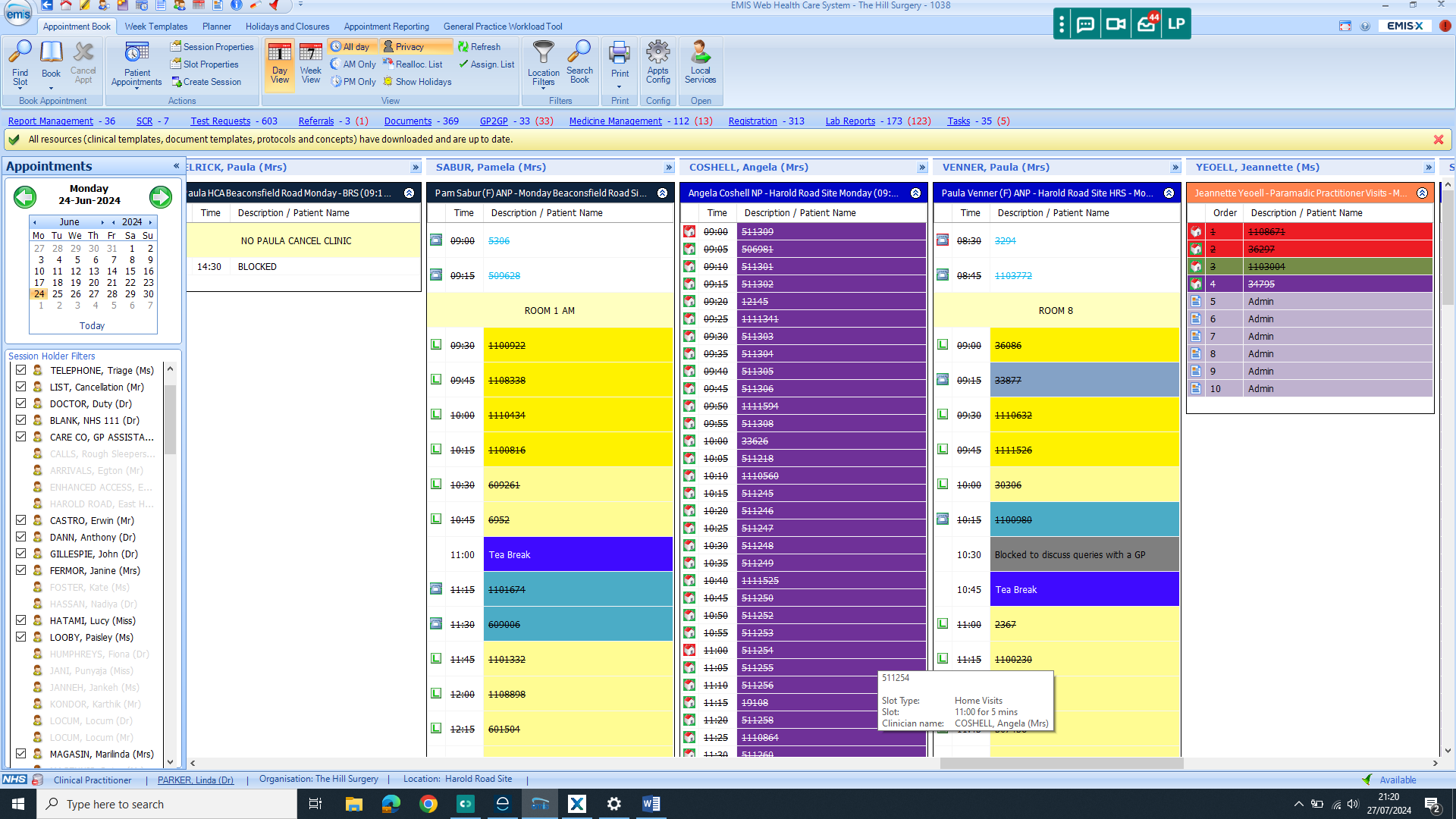
To the second part of the appointment management equation, demand management. This is not just about containing and controlling the allocation of appointments but about allocation safety. It all boils down to Donald Rumsfeld’s “Unknown Unknowns”. If you are not mathematically minded, you may wish to go to the next section.
In 1955 Joseph Luft and Harrington Ingham invented the Johari window, it has been adapted for process model improvement in many fields, including at NASA. This concept really came into the public consciousness with Donal Rumsfeld:
“there are known knowns; there are things we know we know. We also know there are known unknowns; that is to say we know there are some things we do not know. But there are also unknown unknowns—the ones we don’t know we don’t know.”
He was commenting on Iraq and weapons of mass destruction, and this is now also known as the Rumsfeld matrix.
We have used this concept in the development of our triage and appointment allocation system for safe and effective allocation of resource and safety netting.
To labour the point with a booking system:
Patients who phone are:
- The known knowns: patients who booked an appointment and are seen and assessed, we know why they all booked and what is wrong with them.
- The known unknowns: if we logged the names of those who wanted an appointment but did not get one, we did not take any details of the problem, so the problem is unknown. We may be able to deal with them at a later date if capacity allows, they will become Known Knowns. There is an unquantified and qualified health risk until that risk known when the patient is appointed.
- The Unknown Knowns: if we logged the number of patients that wanted an appointment, but did not get one, and we did not take any details, but we know how many patients wanted to be seen, but were not, so we know capacity short fall, but not the health risk. All GP cloud based telephony systems will tell you this.
- Unknown Unknowns: patients who phoned, “I want to see my GP” but no capacity, they did not get an appointment, told to phone back, no details taken or log of the number of callers. We don’t know who they were, why they called, or how many there were. The old system.
So now we come to the Hill Surgery Triage system, making all calls Known Knowns:
- The Known Knowns: The patient calls, they define their problem by answering a series of triage questions. They are placed on the triage list (known capacity for appointments for the day), they are allocated to a clinical list for an appointment for someone to deal with the problem (face to face, phone, visit etc), or to a clinical administrative list depending on the issue. We can prioritise problems that are urgent, serious and need a face to face appointment on the day ie. signs of a possible cancer, over a routine blood pressure check.
- The Known Unknown (how they become a Known Known): The patient calls. There is no space on the triage list, as there is no appointment capacity left, they are given signposting information, and placed on the cancellation list. However, they have defined their problem by answering a series of triage questions. The problem severity and urgency is assessed from the answers to the questions. From the cancellation list they may be booked later in the week, squeezed in on an emergency appointment, redirected to duty doctor, results doctor, clinical administrative doctor, specialist nurse or the medication management team etc.
- The Unknown Known: The patient calls to ask for an appointment, there is no capacity on the triage list, they are unable or unwilling to give any details of their problem. If we can identify them we are able to access their medical record to check for alerts for terminal illness, learning disability, dementia, communication difficulty or a safeguarding concern etc, which may make giving details of their current problem difficult, we can partially assess risk from pre existing knowns, and appoint accordingly to assess further.
- The Unknown Unknown: The patient calls but hangs up before their call is answered or does not answer the call back. This is now a very small percentage, now that most patients have changed security settings to allow call back from a private or withheld number (we operate a cloud based telephone system, so there is no telephone number, as do the majority of GP surgeries).
On any one day there will be 150 – 200 GP or specialist nurse appointments for on the day “GP” calls, Plus the nursing team and the physiotherapists appointments. There will be a similar number on both the cancellation list and the duty doctor administrative and call list, the majority are placed for action somewhere, starting with the most severe or the most vulnerable.
We know the phone messages can be annoying, and answering the triage questions can be exasperating, but we now know:
- how many patients contact us each day,
- who they are,
- what they are contacting us about,
- how we can prioritise severe and urgent problems,
- safety net the calls, and
- how much we can flex our capacity if needed for issues that genuinely can not wait.
So “why can’t I just ask to see a GP like I use to?” because demand always exceeded supply and not bothering to allocate the limited resource on the basis of a risk assessed need rather than personal want is dangerous and medically indefensible in 2024. General practice is the first contact for a suspicion of cancer, diabetes, heart disease and neurodegeneration, we can not turn these patients away because the frequent attender who knows how to access the surgery, and only wanted an ongoing medical certificate or a social chat with their favourite GP and some reassurance about their normal cholesterol, has booked their appointments. If turning the Unknown Unknowns into Known Knowns is good enough for NASA, its good enough for the Hill Surgery.
Did Not Arrive Data:
Having said all of the above, we are still getting 250 patients a month who simply do not come in for their booked appointments. We are going to reactivate our DNA notification and management policy. Although there are genuine reasons why appointments are not attended, the wasting of appointments that could be used by other patients will need to be actively managed to ensure our appointments are not wasted.
Proactive demand management – Frequent attenders:
We have been working with the primary care network (PCN) on identifying our frequent attenders.
It is well known that a high rate of visits to primary care are made by a small proportion of patients. It is recognised that a small 1% of a primary care population can utilise up to 15% of the entire practice activity. This has a huge impact on the care a practice can give. There can be very valid reasons why patients may need to see their GP frequently, such as complex medical illnesses, cancer, or end-of-life care.
The frequency of patient attendances suggests that we may not be meeting these patient’s needs which may be social and emotional, as well as medical, and that means they are having to visit the surgery more. While some chronic illnesses need regular monitoring, often when a patient is frequently seeing their GP it suggests something different is needed for a small group. For example, patients may benefit from being linked to other non-medical organisations that are able to help them to remain independent and manage their lives, including their medical problems, more confidently.
To help us to provide services that meet the needs of all of our patients, we are putting a new process in place to support these patients.
Continuity of care means patient seeing the same members of the clinical team. There is a growing body of evidence showing continuity is beneficial to both patients and GPs. When the GP practice / patient relationship is stronger, patient’s care is often optimised.
We will be working with our identified cohort of 16 patients (excluding cancer and end of life care) which represent less than <0.1% of our population, whom since the start of 2024 in 7 months have had an average of 191 (175 median) contacts per patient with the practice (range 65 to 449 contacts per patient). We are hoping that with intensive proactive work and support with this small cohort of patients, we will help them manage their perceived health care needs better and rationalise their use of general practice resource, and release capacity for improving access for other patients.
Telephones :
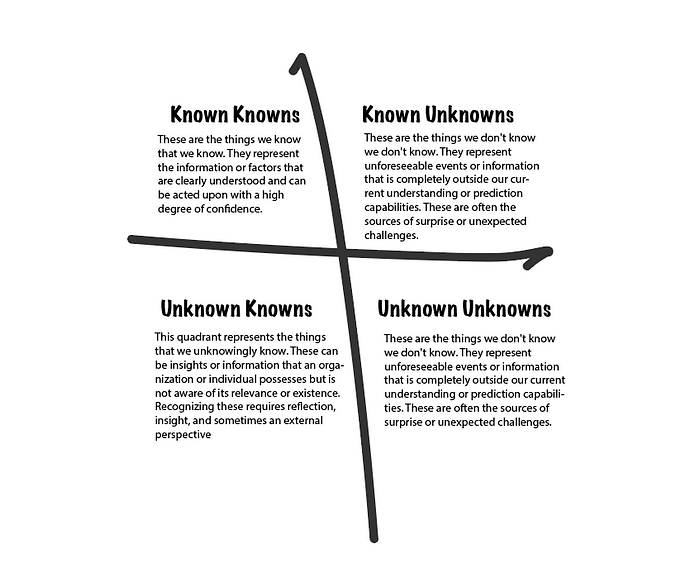
To reassure you that the telephone system is improving, after the call rates doubled at the beginning of the merger, we have analysed the median wait times for answering, remember the call back puts you in the que and you don’t have to wait on the line. Staying on the line wastes of your time and your money with an unnecessary phone bill. The mean average wait times (red) below are affected by the longer wait with increased demand on a Monday morning.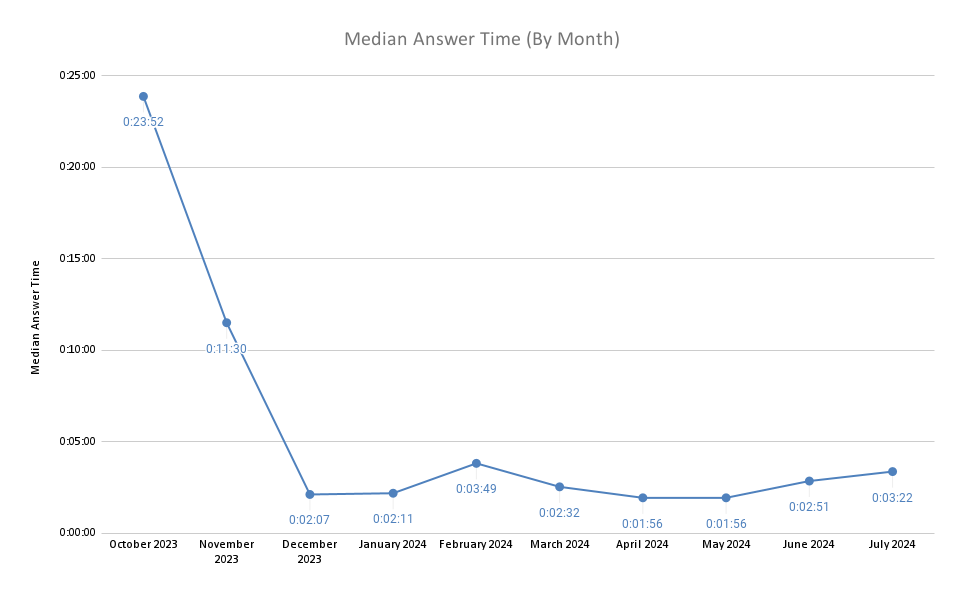
The latest data shows call numbers (posted weekly on the web site) are stabilised at a similar volume to the combined levels of the pre merger surgeries.
Online consultations:
If you can’t face calling, or are rushing off to work, please use the online engage consult. We have expanded capacity for this recently, and it really came into its own when our main clinical system went down with the global windows update problem, we were still able to triage onto this system, and access our document system, so we carried on seeing patients, when many surgeries ground to a halt. The initial registration is a bit involved but once you have set up your account, the access is quite easy. Please access through the website, can be used from phone or computer.
Go to home page of web site, click on the blue “click here” button (computer screen shot, with phone app just scroll down until you see the same multi-coloured box above). There is now a dedicated form for request of medical certificates. This has freed up capacity within the engage in box and they are processed separately from other enquiries or medical consultations.
Practice innovations:
The “Lab Bot” has arrived. A robot computer that helps to file the several thousand individual pathology lab and radiology results we receive each week. Hopefully speeding up the reporting of results. Long in the planning, this MRHA approved protocol driven computer “Lab Bot” was due to be installed the week after the merger, but with all the computer problems post merger and the rapid development of the “Bot’s” capabilities, we did not start trialling it until May. There were some teething problems. The clinical system stability was so poor the “Bot” kept having to be rebooted, but this has been stabilised. “Lab Bot” was put in the “Dog House” when the software engineers managed to programme it to send a normal text message for every individual result. This meant that if you had a blood count for anaemia, because there are more than a dozen parameters, you will have received a text for each one – we sincerely apologise for this, and trust it has settled down. Please tell us if it starts doing this again. There is a lot of refinement going on as we speak and we have limited its functionality at present, but you may see the normal results filed by “GPAutomate”. Results can be viewed on the NHS App.
As an aside to the results, in very recent years, there has been studies to show, that some quite marginally out of range results, in asymptomatic patients, have a small chance of cancer or other diseases. So if you find your iron levels are unexpectedly low or your platelet count is suddenly up, or your liver tests are out of range, you may be offered further tests. There is a very low pick up rate in asymptomatic patients so many patients will be offered tests that prove to be normal, please do not worry excessively if we call you to say we are doing some extra tests. The biggest determinant of an early diagnosis and successful treatment, is an early referral, and that comes from General Practice, so many people are screened, to find the one we need to find.
We will be opening up our list from September, this was capped to help stabilise the merger in October. We will be looking to implement an automated registration computerised robot, “Reg Bot”. This has been developed and tested, and we are confident that it will help streamline this process which is manual at present.
Premises and disability access:
We want to be able to refine our access and allocation model. We currently have 8 TAC groups (Targeted Access Cohorts) that are tagged and notifications pop up when the notes are accessed, so the call management and allocation teams can immediately identify patients with special access needs, care home patients, palliative care patients, etc. If we can have a consensus view on which groups prefer which site, we can TAC the appropriate patients. If there are individual preferences for a site, this can be messaged in a different way , but it is useful if the allocators know where to start if there is no preference expressed.
Survey:
Please follow the link and give your opinion. The more responses we get, the more statistically significant the results. We do not want to make changes that are pushed by a vocal minority to the detriment of the majority. We really value your input.
https://www.surveymonkey.com/r/QYPQXCG
Please be aware this survey will close on the 10th August 2024.